SCC is the second most common type of skin cancer; but the incidence is increasing faster. This is likely due to longer life expectancy in the general population, since SCC tends to be more common in the elderly. SCC’s are also more common on areas that have received long term heavy cumulative sun damage (vs intermittent intense exposure and sunburns with BCC), such as the scalp, ears, forearms and back of hands (men), and lower legs (women).
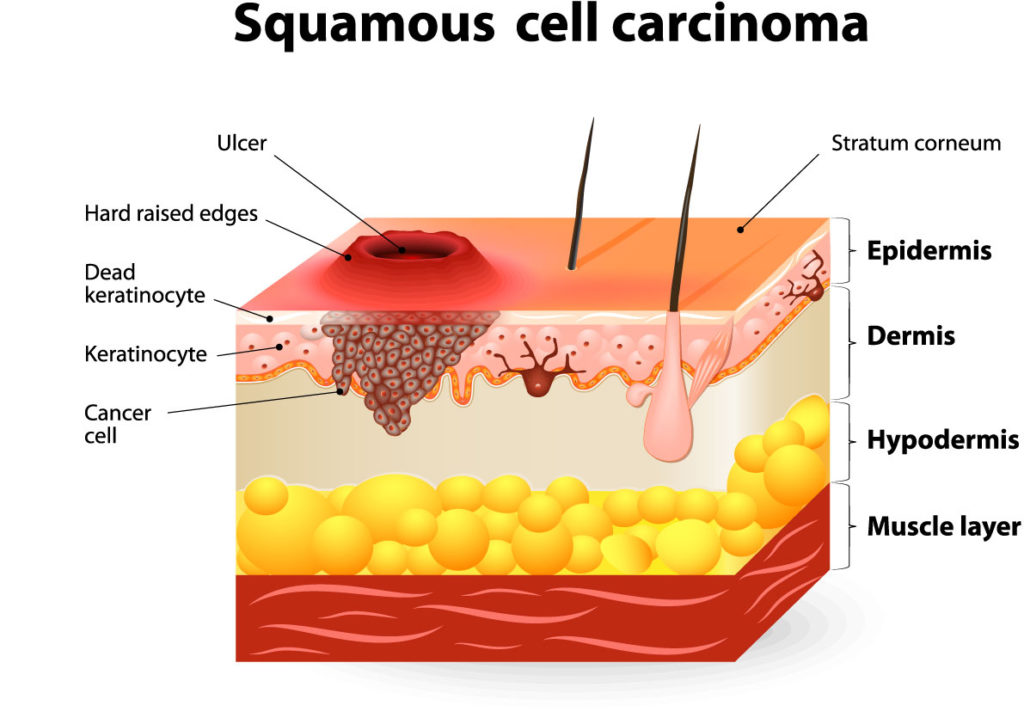
SCC tends to grow faster than BCC, can also invade deeper soft tissue, bone and nearby structures. SCC even has up to a 5% chance of spread (metastasis) to other parts of the body, making treatment and cure difficult.
Typical presentations of SCC:
- a firm, rough, scaly or crusted bump
- a pink rough flat patch or red velvety patch
- non healing ulcer or sore that oozes, crusts, or bleeds (BCC also commonly presents this way)
- a rapidly growing dome shaped lesion with central crater (Keratoacanthoma type SCC)
One final note, SCC can also develop on areas of the body that are not sun-exposed, such as inside the mouth, under the fingernails, or on the genitalia. Using tobacco and underlying hidden infection with HPV (Human papillomavirus or “wart” virus) may play a role in these types of SCC which can be more dangerous and more likely to spread to other parts of the body.